ATD Blog
Lasting Change Versus Check-the-Box Performance Improvement
Fri Jun 11 2021

Without question, performance improvement is critical in healthcare. The financial landscape is changing—perform well and receive a positive payment adjustment or perform poorly and receive financial penalties. Value-based reimbursement is rooted in the quadruple aim: high quality of care, high patient experience of care, low total cost of care, and no care team burnout.
During the last three decades, numerous performance improvement initiatives tested the transition from fee-for-service to value-based payment. These programs require primary care practices, hospitals, and specialists to report quality performance, patient experience of care, and total cost of care data. To avoid negative payment adjustments, healthcare organizations often fall into the endless and unsustainable performance improvement cycle.
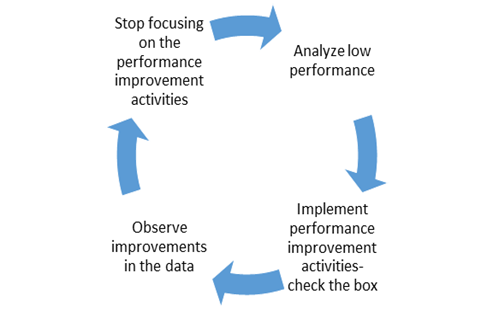
Why do organizations fall into this trap? As long as performance improvement consists of checking a box in the electronic health record that needs to be remembered by each team member, healthcare delivery organizations won’t achieve lasting change. We know the problem, but what can we do about it?
Build in time in every role of the organization for training and testing changes. Don’t just tell staff about a new box. Take the time to get buy-in about the change and show the changes in the context of patient care. Give grace to staff that may take longer in patient care to get the new workflow correct.
Identify a quality improvement (QI) team comprising of representatives for each role in the organization. Each representative should serve as the voice of other staff in the same role. Give every QI team member an equal voice in developing the improvements and space for honest feedback about what works and what doesn’t.
Change electronic HR workflows so that team members don’t have to think about what they will do differently. Using hidden, discrete data fields adds additional clicks. The more time it takes to navigate to the right place, the less likely staff are going to complete the workflow when patient care is busy. Templates and third-party vendors allow organizations to customize documentation workflows that work for them.
Don’t forget training and supporting all staff in the bedside skills that truly improve patient care and clinical outcomes. Improved health outcomes and decreased cost of care require positive patient behaviors and behavior change. It’s worth the time to focus on motivational interviewing competencies, developing patient-driven care plans, and so on.
Data, data, and more data. Quality data in equals quality data out. For example, taking a patient’s blood pressure just as they walked across the entire clinic to get to their exam rooms increases blood pressure levels and the number of patients with high blood pressure. Follow clinical guidelines, wait the five minutes, and get accurate results with better outcomes.
Yes, the above list is exhaustive. Yes, performance improvement and payment reform can be overwhelming. But the message is simple: start slow, use the resources at hand, and lean on the strength and skills of every care team member.
